
Sleep apnea, often relegated to the realm of mere nuisance by its most infamous symptom, snoring, is in reality a clandestine health crisis that afflicts millions worldwide. This condition is characterized by involuntary breathing pauses during sleep, known as apneas, which can occur up to hundreds of times per night in severe cases. These interruptions not only disrupt sleep cycles but also impede the flow of oxygen to vital organs, laying the groundwork for a plethora of potential health complications.
Diving into the basics, sleep apnea manifests in two primary forms: Obstructive Sleep Apnea (OSA), where physical blockages such as relaxed throat muscles hinder air flow, and Central Sleep Apnea (CSA), which results from the brain's failure to send appropriate signals to the muscles that control breathing. A third type, known as Complex Sleep Apnea, emerges when someone exhibits characteristics of both OSA and CSA concurrently. An understanding of these classifications is pivotal in comprehending the multifaceted nature of sleep apnea, as each type demands a distinct approach to diagnosis and treatment.
| Type | Description | Common Treatments |
|---|---|---|
| Obstructive Sleep Apnea (OSA) | Occurs due to physical airway blockage | CPAP machines, lifestyle changes, surgery |
| Central Sleep Apnea (CSA) | Caused by the brain's failure to signal muscles | Adaptive servo-ventilation (ASV), medications |
| Complex Sleep Apnea | A combination of OSA and CSA | Advanced breathing devices, comprehensive treatment plans |
The insidious nature of sleep apnea lies not just in its capability to degrade the quality of life through persistent sleep disruption, but also in its contribution to the development of cardiovascular diseases, hypertension, diabetes, and mental health issues. Early detection and treatment are therefore crucial to mitigating its long-term health repercussions, necessitating increased awareness and understanding of this stealthy malady. Engaging with the specifics of sleep apnea not only illuminates the complexity of this condition but also underscores the importance of adopting a multifaceted strategy for its management and resolution.
Snoring is often the most audible sign of sleep apnea, a condition perceived as benign by many. Yet, it is crucial to understand that this nocturnal nuisance is merely the tip of the iceberg. Beyond the disruptive snoring lie more obscure symptoms that are pivotal in recognizing the complexity and severity of sleep apnea. Instances of observed breathing cessation during sleep, abrupt awakenings accompanied by gasping or choking, and excessive daytime sleepiness despite what appears to be a full night's rest are telltale signs. These manifestations underscore the body's struggle for oxygen, revealing the disorder's stealthy encroachment on an individual's respiratory function.
As we delve deeper, a constellation of symptoms further illuminates the profound impact of sleep apnea. Morning headaches, a sore throat or dry mouth upon awakening indicate the nocturnal efforts and strain. Cognitive impairments, such as difficulties in concentration, mood swings, and irritability, reflect the broader neural and psychological domain that sleep apnea trespasses upon. These symptoms are not standalone nuisances but are interconnected variables that significantly reduce quality of life, signaling an underlying battle with what is sleep disorders.
The identification of these symptoms is critical for the timely diagnosis and management of sleep apnea. Traditional categorizations of sleep apnea, including obstructive, central, and complex, underscore the variety of pathways through which this condition manifests. It's a call to action for both individuals and healthcare professionals to pry beneath the surface of snoring and recognize the multifaceted nature of sleep apnea symptoms.
Understanding these signs is the first step towards confronting sleep apnea—a disorder that is anything but benign. It invites a holistic view of health that not only listens for the sounds of snoring but also perceives the silent signals of distress. It beckons a proactive approach in addressing what is a significant yet surmountable challenge in the realm of sleep disorders, offering a beacon of hope for those ensnared by its grasp.
Diving into the complexities of sleep apnea requires an exploration of its multifaceted causes, revealing a landscape where genetics, lifestyle, and environmental factors intertwine. At its core, sleep apnea occurs when the muscles that support the soft tissues in the throat, such as the tongue and soft palate, temporarily relax, leading to a narrowed airway that interrupts breathing. This phenomenon can be exacerbated by genetic predispositions that influence the structure of the craniofacial region and neck, contributing to a narrower airway. Furthermore, obesity plays a critical role, as excess fat deposits around the neck area can further restrict airway patency, making it one of the leading risk factors for the development of sleep apnea.
In addition to anatomy and body composition, hormonal imbalances and the natural aging process also contribute to the risk profile of what is sleep disorders, including sleep apnea. Hormonal shifts, particularly in the context of conditions such as hypothyroidism or acromegaly, can lead to changes in the airway's structure and muscle tone, increasing vulnerability to apnea events. The aging process itself is accompanied by a loss of muscle tone throughout the body, including the muscles responsible for keeping the airway open, thus heightening the risk of sleep apnea among older adults. These biological factors underscore the importance of a comprehensive assessment in identifying individuals at higher risk.
Navigating through the causative landscape of sleep apnea also brings to light the impact of lifestyle choices and environmental influences. For instance, smoking and alcohol consumption have been linked to an increased risk of sleep apnea due to their effects on airway inflammation and muscle relaxation in the throat, respectively. Additionally, the use of sedatives and certain medications can exacerbate the condition by further decreasing the tone of the muscles in the upper airway. This intricate web of causes highlights the complexity of sleep apnea, underscoring the necessity for an individualized approach to diagnosis and management, taking into account the diverse factors that can predispose someone to this sleep disorder.
Sleep apnea transforms the nocturnal quest for rest into a harrowing ordeal, with ramifications extending far beyond simple fatigue. The cascade of health complications stemming from this sleep disorder elucidates its severity. To start, cardiovascular woes are prominent among those suffering from untreated sleep apnea. The intermittent oxygen deprivation and subsequent stress on the heart can lead to hypertension, arrhythmias, heart attacks, and even stroke. This is predicated on the strain placed on the cardiovascular system each time breathing pauses, heightening blood pressure and forcing the heart to work harder.
Furthermore, the ripple effects of sleep apnea disturb cognitive functions and emotional health. Sufferers often experience diminished concentration, memory lapses, and an increased risk of depression and anxiety. The disruption of sleep architecture, particularly the deep and restorative stages of sleep, hampers the brain's ability to process memories and manage emotions. The resulting daytime drowsiness not only impairs daily functioning but also raises the risk of accidents, particularly while driving.
Metabolic dysregulation is another critical health implication of sleep apnea. Research links the disorder to insulin resistance and type 2 diabetes, underscoring the intricate interplay between sleep quality and metabolic health. The recurrent nighttime awakenings and oxygen fluctuations appear to disrupt glucose metabolism, pushing the body towards a predisposition for diabetes.
Lastly, sleep apnea's impact on lifestyle and quality of life cannot be overstated. The condition exacerbates what is sleep disorders, reducing one's ability to lead an active, healthy life. Chronic fatigue leads to decreased physical activity, while the psychological stress tied to persistent sleep disruption fosters social withdrawal and strained relationships. Thus, understanding and addressing sleep apnea is crucial not just for night-time relief but for safeguarding one's overall health and well-being.
In the realm of sleep disorders, effective management of sleep apnea is crucial for restoring restful sleep and safeguarding long-term health. The cornerstone of therapy often lies in Continuous Positive Airway Pressure (CPAP) machines, which deliver a steady stream of air through a mask to keep the airways open during sleep. This method has been scientifically proven to alleviate symptoms, enhance sleep quality, and reduce the health risks associated with sleep apnea, including hypertension and cardiovascular disease.
Aside from mechanical interventions, dental appliances have emerged as a viable option for those with mild to moderate conditions. These devices, custom-fitted by dental professionals, work by repositioning the jaw or tongue during sleep to keep the airway unobstructed. While not suitable for everyone, they offer a less intrusive alternative to CPAP machines, with research showcasing their effectiveness in reducing apneic episodes and improving sleep patterns.
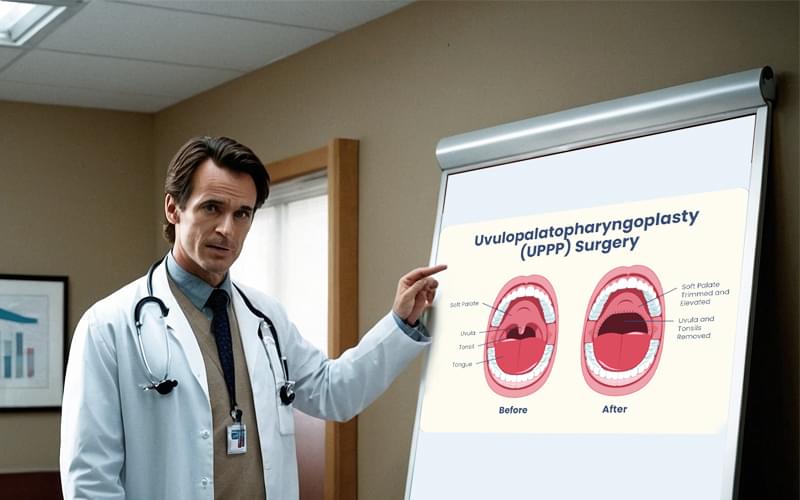
For individuals looking for solutions beyond devices, several surgical options exist, targeting the anatomical contributors to apnea. Procedures such as uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, or maxillomandibular advancement (MMA), which repositions the jaw to enlarge the airway space, can provide long-term relief for selected cases. However, the decision to undergo surgery should be carefully weighed, considering the potential risks and the varying degrees of success.
| Treatment Option | Description | Indicated for |
|---|---|---|
| CPAP Machine | Delivers a steady air pressure to keep airways open | Mild to severe sleep apnea |
| Dental Appliances | Repositions jaw or tongue during sleep | Mild to moderate sleep apnea |
| Surgical Options | Includes procedures like UPPP or MMA to address anatomical causes | Selected cases, depending on anatomical factors |
Conclusively, navigating through the available treatments requires a thorough understanding of the condition and a personalized approach, guided by healthcare professionals. By exploring these options, individuals can embark on a journey towards improved sleep quality and overall health, demonstrating that victory over sleep apnea is within reach.

Combatting sleep apnea extends beyond clinical interventions, venturing into the realm of lifestyle modifications that can significantly ameliorate symptoms and improve overall well-being. A paramount strategy involves weight management; excessive weight, especially around the neck, exacerbates airway obstruction during sleep. Scientific studies underscore the correlation between weight loss and the reduction in sleep apnea severity, suggesting that even a modest reduction in weight can lead to noticeable improvements in sleep quality and a decrease in the apnea-hypopnea index, which measures the severity of sleep apnea.
Equally important is the role of physical activity in the management of sleep apnea. Regular exercise, extending beyond its general health benefits, directly impacts sleep apnea by improving respiratory strength, enhancing heart health, and promoting weight loss. Moreover, activities like yoga that emphasize breath control and respiratory muscle strength can provide specific benefits by improving airway tone and reducing episodes of airway collapse during sleep. It is imperative, however, for individuals to consult healthcare professionals before embarking on exercise programs, ensuring the activities chosen are compatible with their overall health status.

Lastly, dietary adjustments play a crucial role, not only in weight management but also in reducing inflammation and oxidative stress, factors that are pertinent in the pathophysiology of sleep apnea. A diet rich in antioxidants and anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, can support respiratory health and potentially mitigate some of the underlying mechanisms contributing to sleep apnea. Furthermore, minimizing the intake of alcohol and sedatives, which relax the throat muscles and can worsen airway obstruction, is recommended for individuals suffering from this condition. Incorporating these lifestyle tweaks, underpinned by scientific rationale, represents a holistic approach to managing sleep apnea, empowering sufferers to reclaim restful nights and vibrant days.

270 Pine Mountain Rd Ste 5 Hudson NC 28638
(828) 757-8282